
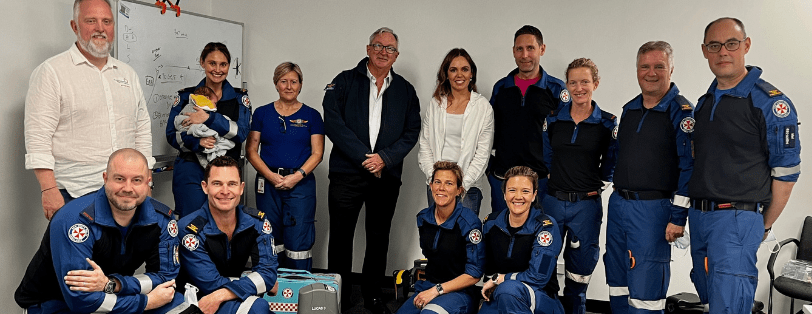
Meet the Team

Natalie Kruit
Chief Investigator, PRECARE
Natalie is a cardiac anaesthetist who did subspecialty training in ECMO at Royal Papworth Hospital (UK), working as one of their ECMO retrieval consultants. She also works as a pre-hospital physician with NSW Ambulance, having done so for the last 11 years. She is the clinical lead and chief investigator for the PRECARE study, having developed the training program and clinical protocol. She is currently undertaking a PhD in advanced cardiac arrest management and optimal service delivery. Natalie is also currently undertaking research in the use of pre-hospital transoesophageal echo for cardiac arrest to optimise forward flow during resuscitation. Her ECPR journey started 10 years ago and she has come to the conclusion that ECPR is just the icing on the cake where cardiac arrest management is concerned. Cardiac arrest is such a heterogenous pathology, making management of each patient interesting as you tailor the ALS to suit the pathology. We must focus on cardiac arrest service delivery and ensure that ALS is meticulously executed in order to get the best outcomes, only then will ECPR work. ECPR can be used to uplift the entire chain of survival and therein lies its true value.
A/Prof Mark Dennis
Chief Investigator, PRECARE
Mark is a Cardiologist at Royal Prince Alfred Hospital specialising in acute heart failure, mechanical circulatory support and cardiac MRI. Mark has an extensive research background having been awarded multiple NHMRC grants, including one for the EVIDENCE trial, a recently completed randomised controlled trial examining expedited vs standard care for refractory cardiac arrest. Mark is currently leading a team looking at the use of mechanical circulatory support during cardiac arrest and cardiac failure. This focusses on patient selection, prognostication and appropriate system design to support patients with cardiovascular failure. Mark’s work in this area of medicine continues to drive system improvement and patient care in the cardiac arrest population. Mark has developed the research protocol for PRECARE and is overseeing the research project.


Andrew Coggins
Andrew’s Field of expertise and interests is in Medical Simulation, Crisis Resource Management and Emergency Medicine
He is driven by a fondness of being at the coal face in Emergency Medicine, but also a deep recognition to have the biggest impact we need to translate our ability professionally into role modelling, teamwork moments, collaboration, coaching and mentoring
His favourite publication is ‘Advances in Simulation’
Brian Burns, Chief Investigator, PRECARE
Emergency Physician, Prehospital and Retrieval Medicine specialist for more than 15 years. Trauma Consultant at RNSH. I believe we will only push the dial in resuscitation outcomes through innovation, research and close attention to marginal gains. Clinician Researcher. Areas of research: cardiac arrest, trauma bleeding and resuscitation. Clinical professor, Faculty of Medicine and Health, Macquarie University and University of Sydney.


Jackie Buckthought
Educator, PRECARE
Jackie has been working as a paramedic for 20 years across 2 services; having spent time in both Victoria and NSW. She has been working in medical retrieval for 5 of those years and feels lucky enough to love what she does everyday. The PRECARE trial has been an incredible opportunity for her to surround herself with colleagues who are passionate about patient outcomes and potentially be part of a revolution in cardiac arrest care in NSW.
Katie Ellis
I’ve been a paramedic for 19 years, currently I work as a Critical Care Paramedic with the Road Retrieval Team in Sydney. Being a part of the PRECARE trial is an amazing and humbling opportunity. Learning the ins and outs of ECMO perfusion and applying that logistically in the prehospital environment has been one of the best learning curves of my career. Being a part of this trial has challenged me clinically and operationally and I’m grateful for every moment we get to push the boundaries and challenge the norms, maybe even pioneering something that will make a difference to a life in the future.


Chris Ennis
I have 27 years of experience in ambulance services—10 in Victoria and 17 in NSW- with the last 8 years in aeromedical road retrieval or on the CareFlight helicopter. ECPR is innovative and ground breaking. It is incredibly exciting to be a part of something that has the potential to change the face of OHCA survival. Medical Teams attending OHCA’s will also undoubtedly lead to further advancements in OHCA management. I am the younger (though not by much) grey haired Chris.
Chris Wilkinson
I’ve been in the ASNSW 42yrs and within Aeromedical for 32 years. My flying career spanned 26 years and I now perform Road Retrievals. I’ve always been at the forefront of Critical Care in Prehospital medicine and firmly believe that ECPR is the next game changer as defibrillation was all those years ago. That’s why I wanted to be part of it and also to challenge myself clinically and professionally.


Karel Habig
I’ve been working in prehospital and retrieval medicine for 20yrs in Australia and overseas. I am committed to bringing critical care to patients as soon as possible after injury or illness wherever they are and prehospital ECMO is the cutting edge of this endevour. To work with such an incredibly skilled and focused clinicians to develop this service has been a highlight of my career.
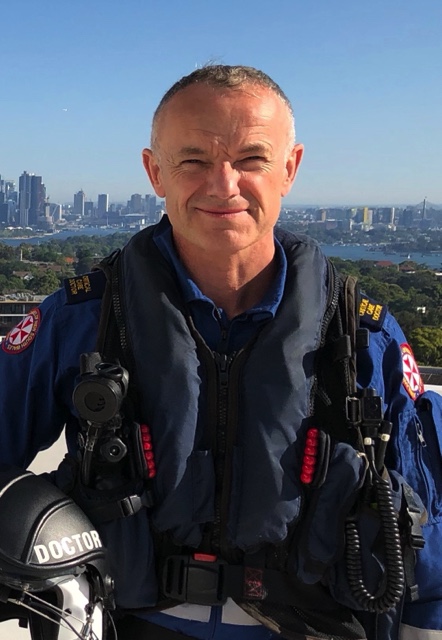
Cliff Reid
Over the last 21 years I have worked as a specialist in emergency medicine, intensive care, and prehospital & retrieval medicine. I have worked for six adult and/or prehospital & retrieval medicine organisations in three countries and have now been with NSW Ambulance for 16 years, where I have been privileged to help advance training and clinical care within the aeromedical service.
I’m thrilled to be part of the PRECARE team, not only to investigate the potential of prehospital ECPR, but also to work with the whole of the Ambulance Service to see how together we can advance the science of cardiac arrest care in general. There is so much we can do to develop a patient-centric approach to cardiac arrest and peri-arrest critical care. At NSW Ambulance we are well placed to embrace this challenge. Let’s go!

Helen Oiver
I have been a consultant anaesthetist for 9 years and have worked in Pre-Hospital and Retrieval Medicine for 7 years in Australia and the UK. PHRM is continually introducing innovative technologies into the pre-hospital environment and advancing patient care in this field, and the introduction of pre-hospital ECPR to the Sydney area is incredibly exciting. To be able to learn this skill and work with such a dedicated and expert team is a privilege and I look forward to seeing the benefits it brings to our cardiac arrest patients.
Neil Ballard
FACEM. Postgraduate year 33, prehospital year 26 – primarily in NSW, but with a few years working in prehospital systems in QLD and the UK.
So much of what we do best in emergency medicine and prehospital & retrieval medicine is starting resuscitation where the patient needs it, regardless of where they are in or out of hospital. Prehospital ECPR epitomises this – for a huge proportion of Sydney, this is the only way to access this potentially life-saving therapy. Working with motivated, skilled friends and colleagues to deliver this is a both challenging and rewarding.
Away from work, life is best spent with family in the ocean or the snow.


Clare Richmond
I’m an emergency physician, who’s worked in PHRM since 2011 in NSW, London and Central Australia. I believe that patients deserve the highest level of critical care, where ever they are located. Having met survivors of ED ECPR, it makes sense to bring it earlier into the patient journey. I’m proud to be part of the team bring this lifesaving intervention and other advanced critical care skills to the patient, wherever they need it.
Ian Ferguson
I’m an emergency medicine and retrieval specialist with a research interest. I’m always keen to investigate new therapies, and to avoid care that doesn’t add meaningful value to patients. PRECARE is an exciting study, allowing us to investigate the use of pre-hospital ECMO, as well as trying to find ways to improve outcomes for all patients suffering treatable cardiac arrests.


Geoff Healy
Geoff is Deputy Medical Manager of SydneyHEMS and has worked with NSW Ambulance since 2007. He was originally a paramedic in NSW Ambulance 25 years ago plus. He is a Consultant Anaesthetist and Director of Trauma at RNSH, and has worked in Prehospital and Retrieval services overseas including London HEMS, Kent Surrey/Sussex and Essex and Herts HEMS.
He is keen to push the edge for patient care in terms of system improvement and innovation, and PRECARE typifies this.
Geoff regularly teaches on the ICP training program and sits on the Clinical Practice Committee at NSW Ambulance.
Malcolm Lau
22 Years experience with NSW Ambulance. I’ve taken advantage of lots of opportunities working as an ICP, ECP, as part of the Special Operations, Education, & Clinical Systems teams over the years.
As I was applying to become an ‘Ambo’. A good friend & experienced paramedic told my mother that I was joining at an exciting time with lots of changes. I thinks prehospital ECPR builds on that for me. I’ve been lucky to see so much innovation in the prehospital arena. I’m excited to be part of another one which sees us, as a multidisciplinary team, successfully bring ECPR to the patient wherever they are located.
I think a random fact about me is that I can be a bit random & disorganised away from work. Which relies on me to use structured approaches to my practice. It drives my wife mad.


Nicolas Shearer
OHCA Desk Clinician. Years in the service: 9 years. Level: ICP
Worked most my years in Western Sydney
To me, Prehospital eCPR means that those patient who could survive OHCA, now have a better opportunity to do.
Chris Partyka
Emergency Physician working in Prehospital & Retrieval Medicine for 9 years.
The introduction of prehospital eCPR provides our patients with equity of access to a life-saving intervention that they otherwise would not have received.
It has been a privilege to be involved in this project which has been both clinically challenging but professionally rewarding.

Prof Hergen Buscher, FCICM, EDIC, DEAA
Senior Staff Specialist, Department of Intensive Care Medicine, St Vincent’s Hospital, Sydney, Conjoint Associate Professor, School of Clinical Medicine, UNSW Medicine & Health, St Vincent’s Clinical Campus, Discipline of Critical Care
- Specialist for Anaesthesia, Intensive Care and Preclinical Emergency Medicine (Germany)
- Specialist for Intensive Care Medicine (Australia)
- Associate Professor University of NSW
- Honorary Professorial Fellow Critical Care Division, The George Institute
- Senior Staff Specialist, St. Vincent’s Hospital, Sydney
- Intensive Care Specialist, St. Vincent’s Private Hospital, Sydney
- Clinical Lead Research, Intensive Care Medicine, St Vincent’s Hospital Sydney
Paul Forrest
Site Principle investigator: RPA
Paul Forrest is head of cardiothoracic anaesthesia and perfusion at Royal Prince Alfred Hospital. He has been involved in ECMO support for more than 30 years, including the development of the NSW ECMO Retrieval Service and the first Sydney trial of ECMO for refractory cardiac arrest.
